In the world of medical billing, accuracy and correct code usage are essential for proper reimbursement and compliance. One of the most frequently misunderstood code types is the X code. If you work in healthcare administration, billing, or coding, understanding X codes can help prevent claim denials and ensure your facility gets paid correctly.
This guide explains what X codes are, when they are used, and how they differ from other medical billing codes.
What Are X Codes?
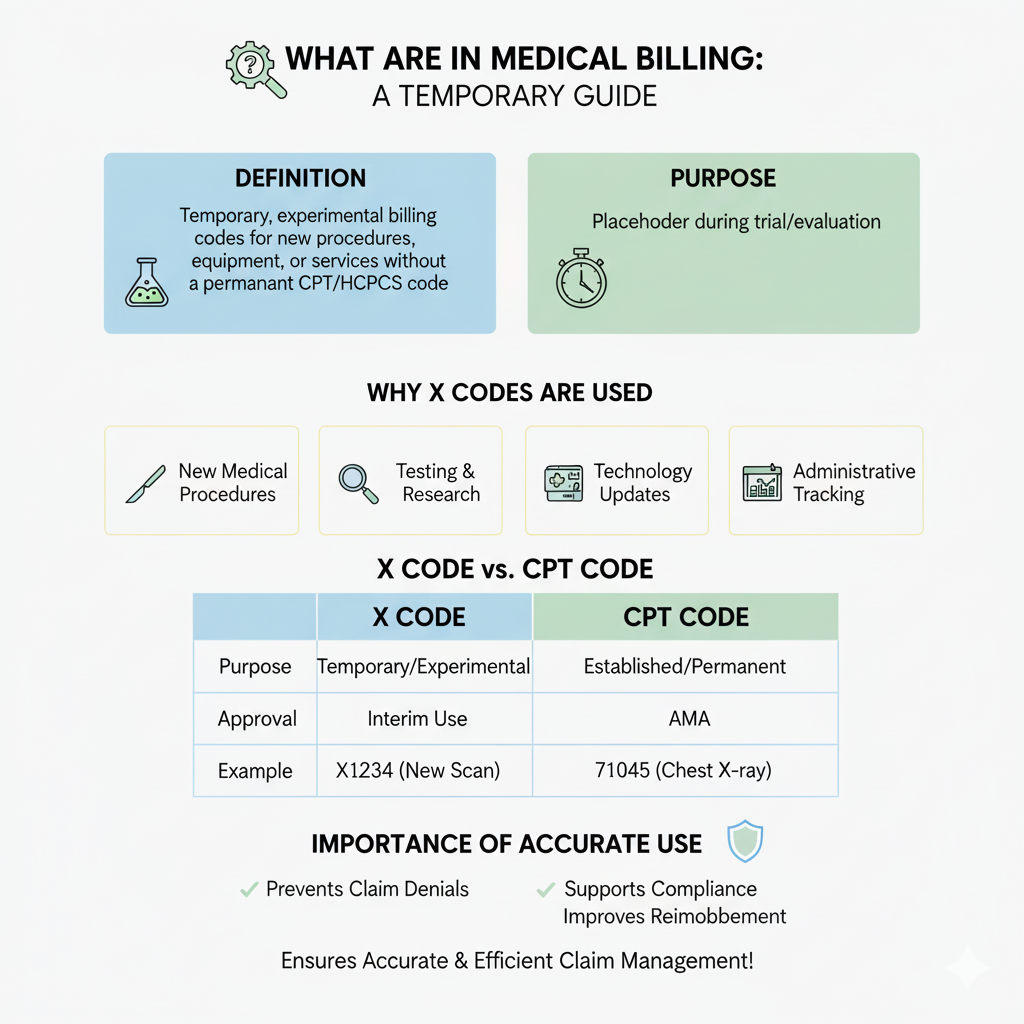
X codes are temporary or experimental billing codes used to identify new medical procedures, equipment, or services that do not yet have a permanent CPT (Current Procedural Terminology) or HCPCS (Healthcare Common Procedure Coding System) code.
They act as a placeholder for new or emerging medical services until the procedure becomes officially recognized and assigned a permanent code. X codes help ensure that providers can still bill and receive reimbursement for these services during the trial or evaluation period.
Why X Codes Are Used
X codes serve several important purposes in medical billing:
- New Medical Procedures:
When a new medical technique or treatment is introduced, it may take time before a CPT or HCPCS code is approved. X codes fill that gap. - Testing and Research:
Services provided during clinical trials or research studies often use X codes for billing and tracking. - Technology Updates:
When new medical devices or diagnostic tools are used that don’t fit existing billing categories, X codes are applied temporarily. - Administrative Tracking:
Payers and billing departments use X codes to monitor utilization of new procedures and assess whether they should become permanent codes.
Example of an X Code
Suppose a hospital introduces a new diagnostic test that’s under evaluation by the Centers for Medicare & Medicaid Services (CMS). Because the test does not yet have a CPT code, the billing department might use a temporary X code such as:
X1234 – Experimental diagnostic imaging procedure
This allows the hospital to document and bill for the procedure while maintaining compliance with billing standards.
Difference Between X Codes and CPT Codes
| Feature | X Code | CPT Code |
| Purpose | Temporary or experimental billing | Established, permanent medical procedures |
| Approval Authority | Issued for interim use | Maintained by the American Medical Association (AMA) |
| Duration | Short-term until official classification | Permanent and regularly updated |
| Example | X1234 – New diagnostic scan | 71045 – Chest X-ray, single view |
In short, X codes are transitional and help bridge the period before a new procedure receives its official CPT or HCPCS classification.
Importance of Correctly Using X Codes
Using X codes accurately is crucial for several reasons:
- Prevents Claim Denials: Proper use of temporary codes ensures claims are not rejected due to incorrect classification.
- Supports Compliance: X codes maintain transparency and accountability during testing or early adoption of procedures.
- Improves Reimbursement Accuracy: Payers can identify and track new services correctly.
- Facilitates Future Coding Updates: Data gathered from X code usage helps coding authorities determine if a new permanent code is needed.
How to Verify and Update X Codes
Billing professionals should always:
- Check with Payers: Verify whether a payer accepts the X code before claim submission.
- Monitor CMS Updates: Temporary codes can change or expire, so keeping up with official updates is essential.
- Maintain Documentation: Properly document all services billed under X codes, including supporting notes and medical necessity.
Regular audits and reviews ensure your practice remains compliant with current medical billing standards.
Conclusion
X codes in medical billing serve as an essential tool for identifying and billing new or experimental medical procedures. They provide a structured way for healthcare providers to seek reimbursement for services that do not yet have established CPT or HCPCS codes.
By understanding when and how to use X codes, billing professionals can ensure accurate claim submission, maintain compliance, and contribute to the evolving landscape of medical billing standards.