CPT/HCPCS code J3301 is a Level II HCPCS drug code used to report triamcinolone acetonide injection, 10 mg. This corticosteroid medication is commonly administered to treat inflammatory conditions, including arthritis, joint pain, allergic reactions, and certain dermatologic disorders.
Because drug dosage, administration method, and payer rules can vary, accurate billing of J3301 is essential to avoid claim denials and ensure correct reimbursement.
Related: ICD-10 Code for Leukocytosis: Complete Coding & Billing Guide
Key Details of CPT/HCPCS Code J3301
| Code | Description | Unit Definition | Common Brand |
|---|---|---|---|
| J3301 | Injection, triamcinolone acetonide, 10 mg | 1 unit = 10 mg | Kenalog (e.g., Kenalog-40) |
Important: J3301 reports only the drug supply, not the procedure used to administer the injection.
How to Calculate Units for J3301
Each billed unit represents 10 mg of triamcinolone acetonide.
Examples:
- 40 mg administered → Bill 4 units of J3301
- 80 mg administered → Bill 8 units of J3301
Always base units on the total dosage actually administered, not vial size.
Steps to Bill CPT Code J3301 Correctly
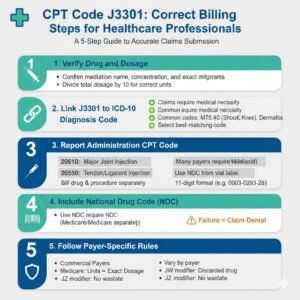
1. Verify Drug and Dosage
Confirm the medication name, concentration, and exact milligrams administered. Divide the total dosage by 10 to determine the correct number of units.
2. Link J3301 to the Correct ICD-10 Diagnosis Code
Claims must include a diagnosis that supports medical necessity. Common ICD-10 codes associated with J3301 include:
- M75.40 – Impingement syndrome of shoulder, unspecified
- M17.9 – Osteoarthritis of knee, unspecified
- L30.9 – Dermatitis, unspecified
Always select the diagnosis code that best matches the clinical documentation.
3. Report the Appropriate Administration CPT Code
Because J3301 is a drug code only, it must be billed in addition to the injection or administration procedure code, such as:
- 20610 – Arthrocentesis/injection of a major joint (e.g., knee, shoulder)
- 20550 – Injection of tendon sheath or ligament
- 96372 – Therapeutic or prophylactic injection (subcutaneous or intramuscular)
Each code should appear on separate claim lines.
4. Include the National Drug Code (NDC)
Many payers, including Medicare and Medicaid, require the NDC number for injectable medications.
- Use the NDC listed on the vial label
- Report it in the required 11-digit format
- Example (Kenalog-40): 0003-0293-28
Failure to report the NDC correctly can result in claim denial.
5. Follow Payer-Specific Billing Rules
Billing requirements may vary by payer:
- Medicare requires units to match the exact dosage administered
Some commercial payers require:
- JW modifier for discarded drug amounts
- JZ modifier when no drug wastage occurs
Always review payer policies before submitting claims.
Example Claim for CPT/HCPCS Code J3301
| Code | Description | Units | Diagnosis | Modifier |
|---|---|---|---|---|
| 20610 | Injection, major joint | 1 | M17.9 | — |
| J3301 | Triamcinolone acetonide, 10 mg | 4 | M17.9 | JW (if applicable) |
Common Billing Mistakes to Avoid
- Billing only 1 unit when more than 10 mg was administered
- Omitting the administration CPT code
- Forgetting to include the NDC number
- Using incorrect or missing JW/JZ modifiers
- Incomplete documentation of dosage or wastage
Avoiding these errors helps reduce denials and audit risk.
Summary: CPT Code J3301 Billing Tips
- 1 unit = 10 mg of triamcinolone acetonide
- Always bill J3301 with an administration CPT code
- Include accurate ICD-10 diagnosis and NDC number
- Apply JW or JZ modifiers when required
- Verify payer-specific guidelines before claim submission
Accurate coding and complete documentation are key to proper reimbursement and compliance.
(FAQs)
1. What is CPT/HCPCS code J3301 used for?
J3301 reports triamcinolone acetonide injection, 10 mg, a corticosteroid used to treat inflammatory conditions such as arthritis, joint pain, allergies, and skin disorders.
2. How many units should I bill for J3301?
Each unit equals 10 mg.
- 40 mg → 4 units
- 80 mg → 8 units
Always bill based on the actual dosage administered.
3. Is an administration code required with J3301?
Yes. J3301 covers only the drug. You must also report the appropriate administration CPT code (e.g., 20610, 20550, or 96372).
4. Is the NDC number required for J3301?
In most cases, yes. Many payers require the NDC from the vial, properly formatted, to process payment.
5. Which modifiers apply to J3301?
- JW – Report when part of the drug was discarded
- JZ – Use when no drug wastage occurred
Documentation must support modifier usage.
6. Is J3301 covered by Medicare?
Yes. Medicare Part B covers J3301 when it is medically necessary and properly documented with:
- Correct units
- NDC number
- Administration CPT code
- Valid ICD-10 diagnosis
7. What documentation is required?
Medical records should include:
- Drug name and strength
- Dosage administered
- Route and site of administration
- Provider signature
- Drug wastage details (if applicable)
8. What is the difference between J3301 and J3300?
Both codes describe triamcinolone acetonide injections, but J3301 represents 10 mg per unit. Always verify the medication strength and NDC before selecting the correct code.
9. How is J3301 reimbursed?
Reimbursement varies by payer and region. Medicare rates are generally based on Average Sales Price (ASP). Check payer fee schedules or CMS drug pricing files for current rates.
Final Note
Correct billing of CPT/HCPCS code J3301 requires careful attention to dosage, documentation, and payer-specific rules. Consistently following best practices helps improve reimbursement accuracy and reduces claim denials.